Observation
Only very few activities performed by health professionals during practical observation and counseling sessions have been done related to maternal nutrition issues, More than 230 major ANC activities and counseling sessions should be conducted, whereas, only less than 40 activities and counseling sessions were done in relation to maternal nutrition from 81 practical observations. On the other hand, food, and nutrition issues were highly neglected by health professionals (Tables 1, 2, and 3).
Table 1 Activities performed by health professionals during practical site observationTable 2 Major non-nutrition related activities performed by health professionalsTable 3 nutrition activities performed by health professionals
For example, what to eat, what to limit to eat, and what not to eat during pregnancy were only counseled to 10, 4, and 5 mothers respectively among 81 practical observations. Nothing is done or said about how to relieve heartburn and constipation. Only one mother had been counseled on how to relieve nausea during the whole observation period of pregnant mothers’ ANC visit.
Most activities and counseling session’s relation to nutrition were related to supplements. Very few clients were informed about what not to eat during pregnancy. The importance of taking fluid during pregnancy was neglected even though it is very essential for both the mother and fetus, Sufficient information had not been provided to mothers about what to limit to eat during their pregnancy (Fig. 1).
Fig. 1
Nutrition related activities performed by health professionals
It is obvious that professionals’ concern is, very few in relation to nutrition. Their main concern is about fetal condition, the health status of the mothers, and the labor history of mothers. They would like to ask the mother gross questions like “what is new?” rather than specific questions about diet and food. On the other hand, we can observe that mothers’ information-seeking behavior is very poor. Only a few questions were raised by pregnant mothers related to nutrition and food. Most questions were relating to their health status and disease condition in addition to their fetal condition. Mothers pay more attention to supplements than food and nutrition. So, nutrition is a neglected subject by the mothers as well (Figs. 2 and 3).
Fig. 2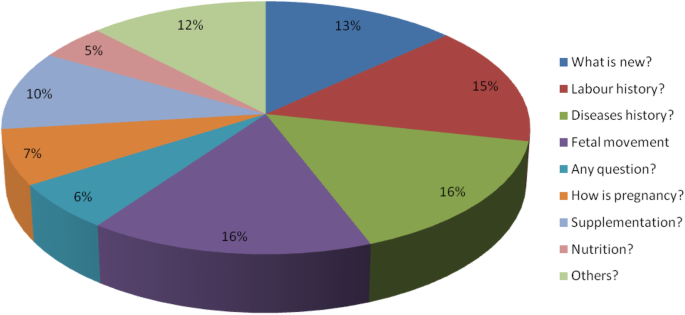
main questions rose by health professionals to mothers
Fig. 3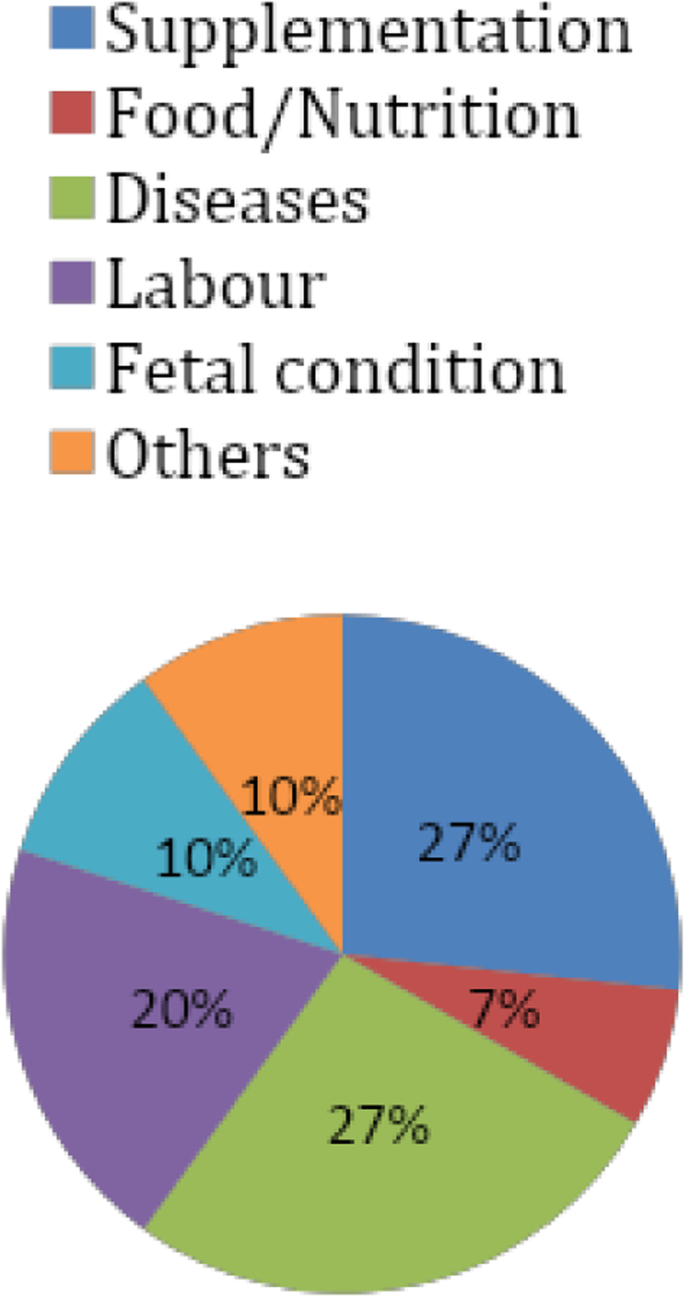
Major questions rose by pregnant mothers to health professionals
From the environmental observation, the majority of the communication channels are wall-mounted displays both in the waiting areas and ANC OPD examination rooms. On the other hand, the majority of the information displayed and transmitted was related to disease conditions and treatment protocols. Many of the messages posted and displayed are less visible from distance. Surprisingly, no information was displayed, and posted in relation to maternal nutrition and diet system. On the other hand, the observer has experienced no nutrition mass-education session during the whole observation period (Tables 4 and 5).
Table 4 Environmental observation of waiting for areasTable 5 Environmental observation of ANC OPD examination rooms
Interview
The interview participants include term pregnant mothers with a mean age of 31 years; the number of pregnancies 2.4 and gestational age 37.8. Most health professionals were males. The two center managers have an average experience of 7 years.
The result of the study is summarized into the following main categories: Adequacy of maternal nutrition, when to provide, where to provide, by whom to be provided, types of information, other sources of information, barriers, and possible solutions of maternal nutrition counseling (Table 6).
Table 6 Profiles of interview participants
Adequacy of maternal nutrition counseling
Most participants respond that maternal nutrition counseling provided to pregnant mothers is inadequate. Among mothers, eight of them replied that maternal counseling provided to them is not adequate; one of them stated that; it is adequate, whereas three of them responded that; maternal nutrition counseling provided by health professionals is fair enough. All health professionals and health center managers responded in the same context and strongly and loudly said; it is difficult to say that maternal nutrition education and counseling provided by health professionals is adequate. They responded that whatever indicator we use, maternal nutrition education and counseling provided during pregnancy couldn’t be stated as adequate. This again has three subcategories:
Time: No or very short time, Content: Most of the study participants responded that; most often gross, less detail and very little maternal nutrition and Mothers’ understanding dimension: Most health professionals responded that since there is very short time allocated to each mother, it is difficult to counsel mothers up to their advanced level of understanding.
“I think the information about nutrition given to us during our ANC visit is fair enough. They told us about our feeding practice. For example, they told us the important food items for the fetus’s growth. They told me how often to eat per day. They told me that the frequency of feeding should be more than the regular time of eating practice” (Interview with pregnant mothers, M3).
“Firstly, I have never given education and counseling about maternal nutrition. I directly came to the institution and told them that I want to have an ANC follow-up and started immediately. But during the whole period of my ANC follow-up, no one gave me the information about nutrition” (Interview with the pregnant mother, M5).
“No information is provided to me about maternal nutrition counseling in my ANC visit from doctors. I didn’t remember anything related to nutrition counseling and education during the whole ANC follow-up” (Interview with pregnant mothers, M7).
“I feel that maternal nutrition education and counseling provided to pregnant mothers is not adequate. Why it is not adequate; one if we see in the respective of time, especially in our setup, for example, we have a lot of clients each day. So it is difficult to tell mothers what to eat, how much to eat, how often to eat per day and other nutrition-related issues” (Interview with senior Gynecologist, P2).
“I don’t think so; it is not adequate. For example, if we measure, according to the time given to nutrition counseling sessions during pregnancy, it is not adequate. To counsel one pregnant mother about everything related to pregnancy, it requires thirty-forty minutes on average. But, in our setup, we counsel each mother for ten-fifty minutes. In our health institution, mothers coming for ANC follow-up have different educational statuses. There are mothers whose educational levels are primary, secondary, and tertiary. Mothers of tertiary educational level have a high understanding capacity for any counseling provided to them. Those of the only primary educational level may have a lower understanding capacity during counseling. Normally, it is important to counsel mothers on what content of food to take like the quantity of carbohydrate, fat, minerals, proteins, vitamins, and water. But, we roughly tell mothers to take vitamins; fluids, protein, and others which only contain gross information. But, it is important to tell the details of these things to mothers. In general, maternal nutrition counseling and education provided to pregnant mothers are not adequate” (Interview with the emergency surgical officer, P6).
“In my opinion, maternal education and counseling service provided by health professionals to pregnant mothers are not adequate. When are we going to measure the adequacy of this service using indicators like time, content, understanding of mothers, and others; for example, if we see regarding time given to nutrition counseling, there are more than 150, clients each day in our health facility. On the other hand, we have only four ANC OPD examination rooms. Having such a huge number of clients and very few health professionals, it is so difficult to offer proper nutrition counseling and education to each mother” (Interview with center manager, CM2).
When to provide it?
Among the eleven mother respondents, six of them said that; it is better to start at the first ANC visit and continue the process of counseling up to the end of pregnancy. Whereas, five of them replied that; it is possible to start at any time and exercise in each ANC visit. Among the health professional respondents, two of them believed that; it is better to start maternal education, and counseling at the preconception period and continue throughout the whole pregnancy period. Seven of these respondents agreed to start counseling and education in the first ANC visit and continue until mothers give birth. Two of the center managers stated that; the service should start at the first ANC visit and shall continue up to the end of pregnancy. Some participants are thinking about having a fixed day of maternal nutrition counseling among the ANC visits. Most others believed in providing mass-education to all mothers collected around waiting for areas in one of the days in a week.
“Okay, nutritional counseling should be started at the time of the first ANC visit. It should be given by the gynecologist in the examination rooms. But, nutritional counseling should be given up to the end of the pregnancy in each ANC visit” (Interview with the pregnant mother, M2).
“This maternal nutrition counseling should be started before conception. Mothers should ask themselves that am I good enough to become pregnant? So, she has to have a complete medical diagnosis and examination. At that time, anemia, malnutrition, and other disorders could be checked” (Interview with a senior gynecologist, P1).
“For the question, when to provide maternal nutrition counseling, it must be offered at any time of mothers’ ANC visit. It is important to deliver this information at any visit of any pregnant woman. At least it is mandatory to give maternal nutrition counseling in the first ANC visit of every pregnant woman. Detail information should be provided to them in the first ANC visit” (Interview with the gynecologist, P3).
Where to provide it?
All the eleven participants responded that; maternal nutrition counseling and education should be provided in ANC OPD examination rooms by the same health professionals who provide other ANC service packages. Four of them underline that; it is best if given in a separate counseling room by the nutritionists. Three of them believe in providing it in an ultrasound room, triage, and waiting areas of the health institution. Among the participants of health professionals, seven of them strongly believed that; it is better to be provided in separate nutrition counseling rooms. Additionally, two of the health professionals agreed to provide it in waiting areas as well as together with other counseling sessions like family planning, HIV/AIDS, and others. Two of the center managers believed to provide the service in a separate room by the nutritionists. One of the center managers strongly underlined that; this service should be provided in every corner by all concerned health professionals to consistently bringing a behavioral change to mothers. On the other hand, some participants believe that; it is possible to provide it is everywhere like offices, market places, churches, and villages.
“Counseling and education of maternal nutrition shall be given by the same doctor in the OPD examination rooms. After investigation of our laboratory result, doctors told our blood type, the fetal condition, ultrasound result, and food items and drinks to be taken and not. If nutrition professionals assigned in a separate room to offer nutrition counseling to mothers, it is the best and most appropriate way of information delivery to mothers” (Interview with the pregnant mother, M6).
We can use a projector and display nutritional issues around waiting areas of health institutions. Project display can assist mothers to discuss each other in waiting areas (Interview with a senior gynecologist, P4).
“It should be provided by all health care professionals at every corner in a consistent manner. Information provided to mothers should be consistent at all corners” (Interview with center manager, CM1).
By whom it should be provided?
Among the eleven participants of pregnant mothers, four of them believed the possibility of providing maternal nutrition counseling by the gynecologists as the full package of ANC services; the other four participants stated the provision of counseling and education by all health professionals working in ANC OPD examination rooms. Four pregnant mothers strongly agreed on the betterment of counseling if provided by nutritionists in separate counseling units. Three mothers stated that; health institutions could deliver the nutritional information in waiting for areas through different means with the assistance of health professionals or without the presence of them. Seven of the health professionals strongly agreed to the provision of maternal nutrition counseling by the nutritionists in separate counseling units. Two of them indicated the possibility of offering this service by the gynecologists in the same ANC OPD examination rooms. On the other hand, two of the health professionals underline the importance of mass-education in waiting areas by any health professional having nutrition training. Two of the center managers believed that; this maternal nutrition counseling should be provided by nutritionists in separate counseling units. (Table 7).
Table 7 When, where, and by whom nutrition counseling should be provided?
“It is better to assign specific nutrition professionals in separate rooms. If nutrition profession is assigned, mothers can access relevant and sufficient information about maternal nutrition during pregnancy” (Interview with a pregnant mother, M8).
‘It is not the gynecologist, the triage, or other health professionals, the nutrition professional herself/himself should provide the appropriate nutritional counseling to mothers. For instance, let me take myself as an example, I don’t have sufficient knowledge as much as nutritionists have about it” (Interview with a senior gynecologist, P2).
“This education and counseling could be better given by health professionals who are educated and trained in nutrition. It is a fact that nutrition counseling and education could be provided by nutrition professionals better than other health professionals. But, it is possible to provide it by other health professionals like gynecologists, nurses, midwives, and others” (Interview with center manager, CM2).
Types of nutrition information to be provided
Almost all the respondents agreed upon the importance of nutrition counseling to both the mother and the fetus. Basic nutrition information should be provided to all pregnant mothers with special attention for the first pregnancy of the first ANC visit.
“I believed that physicians should counsel the mothers how often, and how much to eat. Particularly, how to prevent nausea and vomiting in the first trimester of pregnancy should be informed to mothers by health professionals” (Interview with the pregnant mother, M4).
“At Minimum, we professionals should counsel mothers what to eat, what not to eat, how often to eat, and how much to eat during their ANC visit. This type of counseling does not consider pregnant women with special conditions like who have diabetes, obesity, and other nutrition-related cases” (Interview with a senior gynecologist, P3).
“Counseling should be based on the stage of pregnancy. In the first trimester, nutrition counseling should focus on the prevention and alleviation of certain disorders like nausea, vomiting, constipation, and heartburn which are related to pregnancy. Proper nutrition counseling based on maternal body mass index and fetal weight gains is vital in the reduction of pregnancy-induced maternal and fetal complications. In the second and third trimester, nutrition counseling and education in relation to varying and balanced for the maintenance of maternal health as well as for the growth and development of the fetus” (Interview with a senior gynecologist, M7).
Other sources of nutrition information
This is to mean that source of information to pregnant mothers other than health professionals in health facilities. These could be divided into three basic categories. This again has four subcategories:
Community-based: Information from community members, elderly people, experienced friends, family members, neighbors, partners, peers, traditional birth attendants, and traditional healers are under the category of community-based sources of information.
Institution-based: Books, brochures, free-call centers, pamphlets, posters, projector display, messages through personal cell phone, and TV display in waiting areas are major institutional-based sources of nutrition information other than health professionals.
Media-based: Internet, magazine, mass-media, newspapers, and radio and TV programs are basic information sources for pregnant mothers in addition to health care professionals.
“We can get nutritional information from the internet, from mothers who have previous experience, from reading books and from mass-media. In myself, I have got information from the internet and experienced mothers about maternal nutrition” (Interview with the pregnant mother, M5).
“As I said before, pregnant mothers can get nutrition-related information from their friends, from older people, from their mothers, from traditional healers, from traditional birth attendants, and other community members. Now the time is more globalized, technology-based and there is the ease of internet access. So, mothers can search for information from the internet as well as they can read books” (Interview with a senior gynecologist, P1).
“The other most important way of maternal nutrition information delivery method for me is by using free-call services. We as an organization have a free-call service providing information for clients about family planning, HIV/AIDS, danger signs, and others. These free-call service providers are actually nurses; so, we can train them about nutrition in detail, and they can provide nutrition information to any client calls to free-call center” (Interview with center manager, CM2).
Barriers to maternal nutrition counseling
Almost all the respondents agreed and emphasized that maternal nutrition counseling is totally neglected and forgotten by all stakeholders. According to the respondent’s perspective, there are many interwoven challenges hindering the provision of maternal nutrition counseling by health professionals to pregnant mothers. These barriers can be categorized into four sub-categories.
Institutional Barriers: these are the main challenges from the health institutions’ side.
Professional Barriers: Attitudes of professionals towards mothers’ understanding, the concentration of clinicians on danger signs, and management of other complications neglecting maternal nutrition, poor communication skill of health professionals, lack of knowledge and skill of health professionals as well as negligence and low attention of health professionals.
“I believe that I am not good enough to provide proper maternal nutrition counseling and education to pregnant mothers during their ANC visit” (Interview with a senior gynecologist).
Maternal Barriers: though pregnant mothers need information about nutrition in detail, there are few weaknesses from their side.
Community Barriers: Religion and culture, as well as the provision of non-scientific and harmful nutrition information to pregnant mothers, were the two main barriers according to the respondents who took part in the study. “In my opinion, physicians neglect nutrition counseling issues. They may think that maternal nutrition has no strong impact on the process of pregnancy. On the other hand, a high number of clients and a shortage of time may be the main barrier to maternal nutrition counseling. Since physicians have many clients per day, they ignore nutrition counseling issues”. (Interview with the pregnant mother, M1).
“There are many barriers to provide maternal nutrition counseling. For example, from the health care provider’s side, the communication barrier is one of the main factors that hinder the provision of nutrition counseling. From the health facilities side, shortage of time because of high client flow is one main barrier. The other barrier of health institutions is there is no counseling guideline. From the clients’ side, as I said before, their educational status is one of the major barriers. Fewer acceptances of mothers to the counseling given to them by health professionals may be another barrier. Sometimes, clients may not listen properly to the words of doctors and vice versa. The economic status of mothers is another most important factor. After we deliver nutrition counseling to mothers, they may suffer due to lack of money to purchase the desired food items and supplements prescribed” (Interview with the emergency surgical officer, P6).
“I think the first one is the lack of attention to the subject. Food and nutrition issues are not that much supported by curriculum and training. The effect of this subject is inter-generational. A mother who is malnourished has a high probability of giving malnourished babies. The problem of nutrition recycles itself. So, the impact of nutrition could be on individuals, households, community, and country level. Though its impact is multi-faceted, it does not give due attention to our curriculum and training programs. On the other hand, we think about pregnancy and childbirth; we always consider danger signs and other complications rather than nutritional issues. In general, nutrition as a subject has no priority given by all stakeholders” (Interview with center manager, CM1).
Possible solutions for barriers to maternal nutrition counseling
The possible solutions have been categorized into five subcategories. Institutional, professional, maternal, community, and national levels of solutions are analyzed. Each possible solution should be established and exercised by all stakeholders to bring dramatic changes in maternal nutrition counseling and education process (Table 8).
Table 8 Possible solutions for maternal nutrition counseling
“First, the issue of maternal nutrition counseling and education should be realized and accepted as very essential to mother and then a separate counseling room with appropriate professional should be opened and assigned. It is very crucial if one specific nutrition profession is assigned in separate rooms for maternal nutrition counseling and education. The other most important thing is sending a text message to pregnant mothers through their personal cell phone” (Interview with the pregnant mother, M6).
“As an intervention; when mothers come to ANC visit, they should get appropriate nutrition counseling. Particularly, in their first visit, mothers should get nutrition counseling in a separate nutrition counseling unit. If it is not possible to recruit nutrition professionals, other professionals providing ANC services like gynecologists, midwives, general practitioners, and others should be trained very well to have sufficient nutrition and counseling skills, If possible institutions should give nutrition training periodically. The other thing pressure from religion should be discussed with religious leaders and solved. Another most important is the empowerment of mothers by education, and the economy. To access the recommended diet, during pregnancy, it is vital to have the potential to produce or to purchase food items. “When the economic status of the mother is poor, it is difficult and shameful to counsel about proper nutrition.” “As a gynecologist was not trained and built to have good knowledge of nutrition science and appropriate nutrition counseling skills” (Interview with a senior gynecologist, P2).
“At least as a solution, professionals should get ready to deliver the minimum maternal nutrition counseling within the short allocated period. On the other hand, brochure preparation, and distribution might be one key solution to deliver maternal nutrition information. If possible, a separate nutrition counseling room by nutrition professionals is the best option. But, I think it is difficult to do so. On the job training to professionals who deliver ANC service could be another important solution” (Interview with a gynecologist, P3).
“Professionals should update themselves timely and accordingly better than clients. On the other hand, the number of clients assigned to each professional should be limited. If the numbers of clients assigned to each health professional become limited, professionals can have time to counsel important issues during pregnancy including maternal nutrition. I didn’t remember a nutrition session in postgraduate (specialization) programs. This course was given to us in an undergraduate class in the title “pediatric health and nutrition.” Its emphasis was more on infants, and children’s nutrition, not maternal nutrition. But, it is in general one aspect of the ANC package. So, it is better to have lectured in post-graduate classes (specialization programs). Or on job training could be given to professionals working in the ANC OPD. If on-the-job training is given. It is best for professionals to deliver appropriate and timely nutrition counseling to mothers. Sometimes, mothers may have sufficient availability and accessibility of food; but due to lack of appropriate information about nutrition and diet, they may miss their chance of proper nutrition and appropriate diet systems. Nutrition counseling could be given to each mother, according to their economic status” (Interview with a senior gynecologist, P4).
A Conceptual framework for maternal nutrition counseling drowns from this research (Fig. 4).
Fig. 4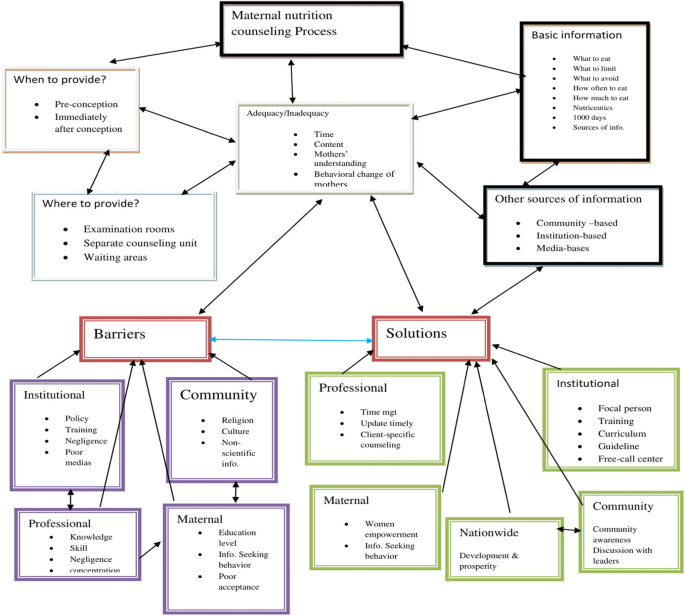
Conceptual framework for maternal nutrition counseling drown from this research
